INTRODUCTION
Periodontal diseases are inflammatory diseases with differing levels of periodontal attachment loss and bone destruction. One of the objectives of periodontal therapy is the morphological and functional regeneration of lost periodontal supporting tissues. Periodontal regeneration requires a sequence of biological events including cell adhesion, migration, proliferation and differentiation [1].
Localized aggressive periodontitis is a distinct entity of periodontal disease and is characterized by deep vertical bony defects that typically affect the first molars and incisors of young patients. Aggressive periodontitis has been defined using the following criteria: 1) age of onset, 2) distribution of lesions, 3) severity of destruction, 4) rate of progression, and 5) response to therapy. A positive family history has also been reported for aggressive periodontitis. Therapy is usually aimed at reducing the pathogenic microflora through scaling and root planing and the administration of systemic antibiotics. However, conservative periodontal therapy may result in reparative wound healing with limited regeneration of the lost tissues. Periodontal surgery combined with platelet-rich plasma and bioactive glass has been introduced as a method to promote regeneration of the lost periodontium and has been studied extensively in the treatment of chronic periodontitis. This case report describes the treatment of a 27-year-old female patient displaying severe localized aggressive periodontitis with documented disease progression. After initial therapy consisting of scaling and root planing and systemic administration of tetracycline, the vertical defects were treated by access flap combined with application of platelet-rich plasma and bioactive glass. Clinical and radiographic findings are reported for up to 9 months after initial therapy, indicating good efficacy of the therapeutic strategy and stability of the treatment outcome.
CASE-HISTORY:
An apparently healthy 27 yr old female patient reported to the Department of Periodontics, D.A.P.M R.V.Dental College-Bangalore with the chief complaint of food lodgement in the upper right back tooth region since 2 years. Occasionally, bleeding occurred while brushing teeth. Patient also gave a family history of her mother losing all her teeth at an early age due to mobility of teeth.
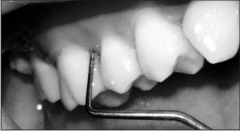
On clinical examination, the oral hygiene status of the patient was found to be good with moderate gingivitis (figure 1). Periodontal examination revealed periodontal
 | Fig 1
 |
pockets in multiple areas with deep pockets (ranging 6-9mm) in first molars (figure 2) in all quadrants and upper central incisors.
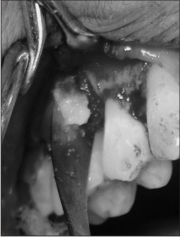
 | Fig 2
 |
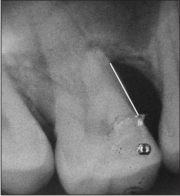
Investigations carried out were (i) Routine haematological investigations which were found to be within the normal ranges. (ii) Radiographs- full mouth Intra-oral periapical radiographs and Orthopantomograph(OPG). OPG showed vertical bony defects in 16, 26, 34, 35, 36, 46, and 47 tooth region (figure 3).
 | Fig 3
 |
(iii) Vitality test was done for 16 tooth which was found to be vital.
Based on the history, clinical and radiographic examinations, and the criteria given by Tonetti and Mombelli et al., a diagnosis of Localized aggressive periodontitis was reached upon.
The treatment plan consisted of-
I. Scaling and root planing.
ii. Systemic administration of tetracycline hydrochloride 250mg four times daily for 14 days.
iii. Patient was recalled 6 weeks after phase-I therapy and at re-evaluation, probing pocket depth was found to be deepest in 16 tooth region with measurement of 7mm. Thereby surgical intervention was deemed necessary and open flap debridement with regeneration using a combination of Platelet rich plasma (PRP) and Bone graft (BG)-Perioglass was planned in relation to 16 tooth region.
Surgical Procedure consisted of the following steps:
a) Preparation of PRP
b) Open flap debridement and
c) Placement of PRP mixed with Perioglass.
Step-1: Preparation of PRP [8]. (Figure 4)
 | Fig 4
 |
1. Briefly, 8 ml of blood was drawn by venipuncture of the antecubital vein. Blood was collected in a sterile tube containing an anticoagulant to avoid platelet activation and degranulation.
2. The first centrifugation is called “soft spin”, which allows blood separation into three layers, namely bottom-most RBC layer (55% of total volume), topmost acellular plasma layer called PPP (40% of total volume), and an intermediate PRP layer (5% of total volume) called the “buffy coat”.
3. Using a sterile syringe, the operator transferred PPP, PRP and some RBCs into another tube without an anticoagulant.
4. This tube underwent a second centrifugation, which was longer and faster than the first, called “hard spin”. This allows the platelets (PRP) to settle at the bottom of the tube with a very few RBCs, which explains the red tinge of the final PRP preparation. The acellular plasma, PPP (80% of the volume), is found at the top.
5. Most of the PPP is removed with a syringe and discarded, and the remaining PRP is shaken well and is ready for use.
6. This PRP is then mixed with Perioglass.
On exposure, a combination defect was found in relation to 16 tooth with 3walled defect apically and 2walled defect coronally (figure 5).
 | Fig 5
 |
Step-3: PRP was mixed with perioglass and placed in the bony defect (figure 6).
 | Fig 6
 |
Following placement of the PRP and Perioglass combination, the defect was closed with interrupted sutures and a periodontal dressing was placed.
Following the surgery, patient was recalled once a month for 9 months. At 9 months recall visit, the probing pocket depth was reduced to 3 mm from a pre-operative measurement of 7 mm in the operated area. (figure 7, 8). Radiographically a defect fill of approximately 60-70% was achieved.
 | Fig 7
 |
 | Fig 8
 |
DISCUSSION
The use of polypeptide growth factors (PGFs) to regulate biological events affecting surgical outcome has recently attracted the attention of researchers [1, 2, 3]. Among all PGFs, platelet derived growth factor (PDGF) and transforming growth factor (TGF-α) have been studied most extensively. PDGF and TGF-α have been shown to promote cell growth, differentiation and periodontal regeneration [2, 3, 4]. Platelet derived growth factor (PDGF) and TGF-α are abundant in the alpha granules of platelets [5] and platelets are involved in the wound-healing process and represent a natural source of PGFs [3]. A convenient approach to obtain autologous PDGF and TGF-α is the use of platelet-rich plasma (PRP) that can be easily prepared from patient’s own blood by centrifugation [6, 7]. It can be rationalized that by increasing local concentrations of PGFs with the application of PRP, the periodontal healing outcome would be enhanced.
The addition of PRP to bone grafts or guided tissue regeneration (GTR) has been shown to significantly enhance gain in clinical attachment when compared to the control groups of bone grafts, GTR or open flap debridement alone in intra-bony periodontal defects [9–14]. Only in one study including GTR in the control group, the clinical results failed to demonstrate the superiority of the combined approach with PRP. However, the authors found positive effects on the soft and hard tissue healing [15].
Despite the fact that pre-clinical and initial clinical data appear promising, it is not possible to draw definitive conclusions at this time. In this process, trials evaluating the efficacy of PRP in combination with different regenerative materials can still add valuable information for the clinician in decision making regarding effective and predictable treatment alternatives for periodontal regeneration especially in aggressive periodontitis patients which are difficult to manage clinically because of the destructive and progressive disease character seen in young individuals.
REFERENCES
1. Giannobile WV. The potential role of growth and differentiation factors in periodontal regeneration. J Periodontol 1996; 67:545–553.
2. Howell TH, Fiorellini JP, Paquette DW, Offenbacher S, Giannobile WV, Lynch SE. A phase I/II clinical trial to evaluate a combination of recombinant human-derived growth factor-BB and recombinant human insulin-like growth factor-I in patients with periodontal disease. J Periodontol 1997; 68:1186–1193.
3. Giannobile WV, Somerman MJ. Growth and amelogenin like factors in periodontal wound healing. A systematic review. Ann Periodontol 2003; 8:193–204.
4. Oates TW, Rouse CA, Cochran DL. Mitogenic effects of growth factors on human periodontal ligament cells in vitro. J Periodontol 1993; 64:142–148.
5. Assoian RK, Grotendorst GR, Miller DM, Sporn MB. Cellular transformation by coordinated action of three peptide growth factors from human platelets. Nature 1984; 309: 804–806.
6. Marx RE, Carlson ER, Eichstaedt RM, Schimmele SR, Strauss JE, Georgeff KR. Platelet-rich plasma. Growth factor enhancement for bone grafts. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1998; 85:638–646.
7. Okuda K, Kawase T, Momose M, Murata M, Saito Y, Suzuki H, et al. Platelet-rich plasma contains high levels of platelet-derived growth factor and transforming growth factor-α and modulates the proliferation of periodontally related cells in vitro. J Periodontol 2003; 74:849–857.
8. Raja SV, Naidu ME. Platelet rich fibrin- Evaluation of second generation platelet concentrate. Indian Journal of Dental Research, 2008; 19(1): 42-46
9. De Obarrio JJ, Arauz-Dutari JI, Chamberlain TM, Croston A. The use of autologous growth factors in periodontal surgical therapy: Platelet gel biotechnology-case reports. Int J Periodontics Restorative Dent 2000; 20:487–497.
10. Lekovic V, Camargo PM, Weinlaender M, Vasilic N, Kenney EB. Comparison of platelet-rich plasma, bovine porous bone mineral, and guided tissue regeneration versus platelet-rich plasma and bovine porous bone mineral in the treatment of intrabony defects: A re-entry study. J Periodontol 2002; 73:198–205.
11. Kotsovilis S, Markou N, Pepelassi E, Nikolidakis D. The adjunctive use of platelet-rich plasma in the therapy of periodontal intraosseous defects: a systematic review. J Periodont Res 2010; 45: 428–443.
12. Camargo PM, Lekovic V, Weinlaender M, Vasilic N, Madzerevic M, Kenney EB. A re-entry study on the use of bovine porous bone mineral, GTR, and platelet-rich plasma in the regenerative treatment of intrabony defects in humans. Int J Periodontics Restorative Dent 2005; 25:49–59.
13. Hanna R, Trejo PM, Weltman RL. Treatment of Intrabony defects with bovine-derived xenograft alone and in combination with platelet-rich plasma: A randomized clinical trial. J Periodontol 2004; 75:1668–1677.
14. Okuda K, Tai H, Tanabe K, Suzuki H, Sato T, Kawase T, et al. Platelet-rich plasma combined with a porous hydroxyapetite graft for the treatment of intrabony periodontal defects in humans: A comparative controlled clinical study. J Periodontol 2005; 76:890–898.
15. Christgau M, Moder D, Wagner J, Gla BM, Hiller K-A, Wenzel A, et al. Influence of autologous platelet concentrate on healing in intrabony defects following guided tissue regeneration therapy: a randomized prospective clinical split-mouth study. J Clin Periodontol 2006; 33:908–921.
|